辅酶Q 10 (Coenzyme Q 10)
产品简介
辅酶Q10是一种类维生素化合物,参与机体细胞能量的生成。 机体细胞内辅酶10的水平随着年龄增长而降低。 因此老年人似乎更缺乏这种化合物。 根据临床医学报道,充血性心力衰竭,高血压,牙周病,糖尿病,帕金森病,某种肌肉疾病和艾滋病等可能与较低水平的辅酶Q10有关。*
造成辅酶Q10缺乏的其他原因,包括:
- 营养缺乏,如维生素B6缺乏症
- 辅酶Q10合成或利用环节的遗传缺陷
- 由于疾病导致的组织需求增加
- 线粒体疾病
- 由于衰老导致的氧化应激
- 他汀类药物治疗的副作用
研究表明,辅酶Q10在体内起着几个关键作用。辅酶Q10的主要功能是帮助细胞产生能量,参与制备三磷酸腺苷(ATP),参与细胞内的能量转移。它的另一个关键作用是作为抗氧化剂,保护细胞免受氧化损伤。辅酶Q10存在于身体的每个细胞中,能量需求越大的器官辅酶Q10的含量就越高,如心脏,肾脏,肺和肝脏。*
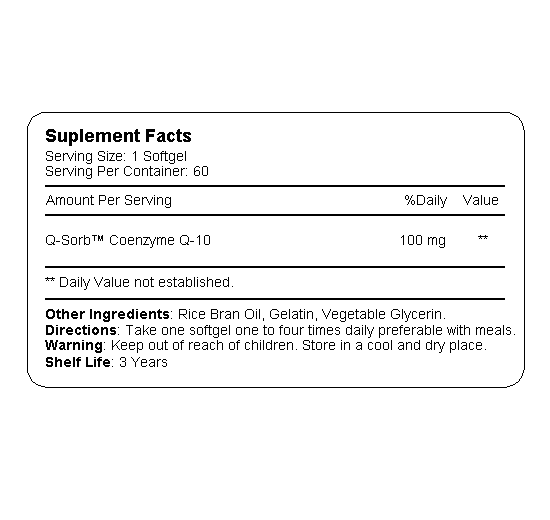
研究表明,服用外源性辅酶Q10可以提高血浆中辅酶Q10的含量。 CoQ10的标准剂量范围是每天90mg至200mg,剂量在高达500毫克时似乎耐受良好,一些研究使用甚至更高的剂量,没有任何严重的副作用。辅酶Q10是一种脂溶性化合物,其吸收缓慢且有限。然而,服用辅酶Q10膳食补充剂可以帮助机体提高辅酶Q10的吸收速度,服用辅酶Q10者比未服用者的吸收速度快三倍。我们的身体不存储辅酶Q10,因此,长期服用受益更多。*
更多专业研究请参阅《临床研究》
本产品诚招经销商和批发商
- * 本声明未经美国食品药品管理局评估。 本产品不用于诊断,治疗或预防任何疾病。 本网站提供的信息仅供您一般参考,不能代替专业医疗建议或针对特定疾病的治疗。
临床研究
Here, you can read some of important published clinical research papers about CoQ 10 which support heart health. Published peer reviewed studies can be accessed through PubMed at www.ncbi.nlm.nih.gov/pubmed. For more information, please contact Renylin Bio-Health Inc
The level of CoQ 10 decrease with age
Age-related Changes in the Lipid Compositions of Rat and Human Tissues
In human pancreas and adrenal the ubiquinone content was highest at one year of age, whereas in other organs the corresponding peak value was at 20 years of age, and was followed by a continuous decrease upon further aging. A similar pattern was observed in the rats, with the highest concentration of ubiquinone being observed at 30 days of age.
Source: LIPIDS, Vol. 24, No. 7 (1989)
Coenzyme Q10:An Independent Predictor of Mortality in Chronic Heart Failure

Coenzyme Q10 An Independent Predictor of Mortality
in Chronic Heart Failure
Objectives The aim of this study was to investigate the relationship between plasma coenzyme Q10 (CoQ10) and survival in patients with chronic heart failure (CHF).
Background Patients with CHF have low plasma concentrations of CoQ10, an essential cofactor for mitochondrial electron transport and myocardial energy supply. Additionally, low plasma total cholesterol (TC) concentrations have been associated with higher mortality in heart failure. Plasma CoQ10 is closely associated with low-density lipoprotein cholesterol (LDL-C), which might contribute to this association. Therefore we tested the hypothesis that plasma CoQ10 is a predictor of total mortality in CHF and could explain this association.
Methods Plasma samples from 236 patients admitted to the hospital with CHF, with a median (range) duration of follow-up of 2.69 (0.12 to 5.75) years, were assayed for LDL-C, TC, and total CoQ10.
Results Median age at admission was 77 years. Median (range) CoQ10 concentration was 0.68 (0.18 to 1.75) mol/l. The optimal CoQ10 concentration for prediction of mortality (established with receiver-operator characteristic [ROC] curves) was 0.73 mol/l. Multivariable analysis allowing for effects of standard predictors of survival—including age at admission, gender, previous myocardial infarction, N-terminal peptide of B-type natriuretic peptide, and estimated glomerular filtration rate (modification of diet in renal disease)—indicated CoQ10 was an independent predictor of survival, whether dichotomized at the ROC curve cut-point (hazard ratio [HR]: 2.0; 95% confidence interval [CI]: 1.2 to 3.3) or the median (HR: 1.6; 95% CI: 1.0 to 2.6).
Conclusions Plasma CoQ10 concentration was an independent predictor of mortality in this cohort. The CoQ10 deficiency might be detrimental to the long-term prognosis of CHF, and there is a rationale for controlled intervention studies with CoQ10.
Source: Molyneux et al.JACC Vol.52, No. 18, 2008:1435–41
Coenzyme Q10 in the treatment of hypertension

Coenzyme Q10 in the treatment of hypertension:
a meta-analysis of the clinical trials
Our objective was to review all published trials of coenzyme Q10 for hypertension, assess overall efficacy and consistency of therapeutic action and side effect incidence. Meta-analysis was performed in 12 clinical trials (362 patients) comprising three randomized controlled trials, one crossover study and eight open label studies. In the randomized controlled trials (n¼120), systolic blood pressure in the treatment group was 167.7 (95% confidence interval, CI: 163.7–171.1) mmHg before, and 151.1 (147.1–155.1) mmHg after treatment, a decrease of 16.6 (12.6–20.6, Po0.001) mmHg, with no significant change in the placebo group. Diastolic blood pressure in the treatment group was 103 (101–105) mmHg before, and 94.8 (92.8–96.8) mmHg after treatment, a decrease of 8.2 (6.2–10.2, Po0.001) mmHg, with no significant change in the placebo group. In the crossover study (n¼18), systolic blood pressure decreased by 11 mmHg and diastolic blood pressure by 8 mmHg (Po0.001) with no significant change with placebo. In the open label studies (n¼214), mean systolic blood pressure was 162 (158.4–165) mmHg before, and 148.6 (145–152.2) mmHg after treatment, a decrease of 13.5 (9.8–17.1, Po0.001) mmHg. Mean diastolic blood pressure was 97.1 (95.2–99.1) mmHg before, and 86.8 (84.9–88.8) mmHg after treatment, a decrease of 10.3 (8.4–12.3, Po0.001) mmHg. We conclude that coenzyme Q10 has the potential in hypertensive patients to lower systolic blood pressure by up to 17 mmHg and diastolic blood pressure by up to 10 mmHg without significant side effects.
Source: Journal of Human Hypertension (2007) 21, 297–306. doi:10.1038/sj.jhh.1002138;
Effects of Coenzyme Q10 in Early Parkinson

Effects of Coenzyme Q10 in Early Parkinson Disease
Evidence of Slowing of the Functional Decline
Conclusions: Coenzyme Q10 was safe and well tolerated at dosages of up to 1200 mg/d. Less disability developed in subjects assigned to coenzymeQ10 than in those assigned to placebo, and the benefit was greatest in subjects receiving the highest dosage. Coenzyme Q10 appears to slow the progressive deterioration of function in PD, but these results need to be confirmed in a larger study.
Source: Arch Neurol. 2002;59:1541-1550
Atorvastatin Decreases the Coenzyme Q10 Level in the Blood of Patients

Atorvastatin Decreases the Coenzyme Q10 Level in the Blood of Patients at Risk for Cardiovascular Disease and Stroke
Background: Statins (3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitors) are widely used for the treatment of hypercholesterolemia and coronary heart disease and for the prevention of stroke. There have been various adverse effects, most commonly affecting muscle and ranging from myalgia to rhabdomyolysis. These adverse effects may be due to a coenzyme Q10 (CoQ10) deficiency because inhibition of cholesterol biosynthesis also inhibits the synthesis of CoQ10.
Conclusions: Even brief exposure to atorvastatin causes a marked decrease in blood CoQ10 concentration. Widespread inhibition of CoQ10 synthesis could explain the most commonly reported adverse effects of statins, especially exercise intolerance, myalgia, and myoglobinuria.
Source: Arch Neurol. 2004;61:889-892
精选问答
辅酶Q10(Coenzyme Q10),也称为泛醌,有时缩写为Q10。这种类维生素的脂溶性物质分布于所有真核细胞中,主要存在于细胞的线粒体中。它是电子传递链的一个组成部分,参与有氧细胞呼吸,以ATP的形式产生能量。人体百分之九十五的能量是以这种方式产生的。 因此,对能量需求最大的器官,例如心脏,肝脏和肾脏,它们的CoQ10含量也最高。
目前医学界普遍认为:辅酶Q10具有提高人体免疫力、增强抗氧化、延缓衰老和增强人体活力等功能,医学上广泛用于心血管系统疾病。*
人体百分之九十五的能量是依靠辅酶Q10的参与产生的,人体细胞和组织离开能量的供给无法生存,尤其对于能耗高的器官,心脏、大脑和肝肾的影响更为严重。随着年龄的增长,体内辅酶Q10的含量会明显下降。 某些疾病,如心脏病,充血性心力衰竭,高血压,牙周病,糖尿病,帕金森病,某些肌肉疾病和艾滋病,都与辅酶Q10水平较低有关。*
造成辅酶Q10缺乏的其它一些原因包括:
- 营养缺乏,如维生素B6缺乏症
- 辅酶Q10合成或利用环节的遗传缺陷
- 由于疾病导致的组织对辅酶Q10的需求增加
- 线粒体疾病由于衰老导致的氧化应激
- 服用他汀类药物的副作用
辅酶Q10存在于肉类,鱼类和全谷物中。 然而,在这些膳食来源中发现的辅酶Q10的量不足以显着增加体内辅酶Q10水平。
对辅酶Q10进行的大量医学研究表明::
- 心脏病:辅酶Q10已被证明可以改善充血性心力衰竭的症状。CoQ10可能有助于降低血压。一些研究还表明,当与其他营养素结合使用时,辅酶Q10可能有助于已经进行过旁路和心脏瓣膜手术的人的康复。
- 帕金森:早期的研究表明,大剂量的辅酶Q10可能对这种影响运动神经系统疾病的早期阶段的患者有益。
- 他汀类药物引起的肌病:一些研究表明辅酶Q10可能有助于缓解肌肉无力,有时与服用他汀类药物有关。偏头痛。一些研究表明辅酶Q10可能会减少这些头痛的频率。
- 体能表现:由于辅酶Q10参与能量生产,因此相信这种补充剂可能会改善您的体能表现。
内容引自美国梅奥诊所官方网站:www.mayoclinic.org
CoQ10的理想剂量尚未确定。 试验研究中成人的使用剂量为50毫克至1,200毫克/日,有时在一天内分次服用。 典型的日剂量为100毫克至200毫克。详细情况请咨询您的家庭医生。
辅酶Q10的标准剂量范围为每天100mg至200mg。 剂量高达500毫克似乎耐受良好,一些研究使用甚至更高的剂量,没有任何严重的副作用。
因为辅酶Q10是一种脂溶性化合物,其吸收缓慢且有限。 然而,服用辅酶Q10膳食补充剂可以帮助你的身体加快吸收辅酶Q10,服用Q10膳食补充剂比不服用者的吸收速度快三倍。
此外,溶解形式的辅酶Q10,或辅酶Q10和油的组合,可以改善其吸收。
我们的身体不存储辅酶Q10。 因此,长期持续使用辅酶Q10以获得其益处。
补充辅酶Q10似乎对人类具有良好的耐受性。 事实上,一些研究的参与者表明,每天服用1,200毫克16个月没有出现重大副作用。
上述内容引自:www.healthline.com
- * 本声明未经美国食品药品管理局评估。 本产品不用于诊断,治疗或预防任何疾病。 本网站提供的信息仅供您一般参考,不能代替专业医疗建议或针对特定疾病的治疗。